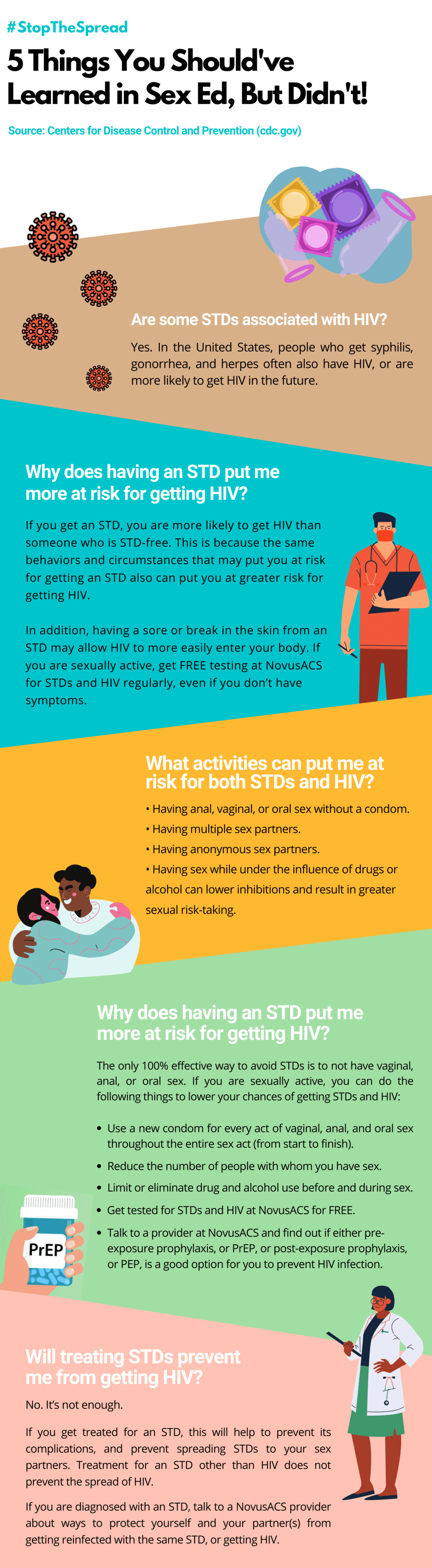
Sexual health is important. But sometimes it’s hard to know exactly what to do or where to go to protect yourself. Don’t worry, we can help. We’ve put together a list of everything you need to know about getting regular HIV/STD tests.
HIV testing should be part of your routine preventative care. If you’re sexually active, you should be getting tested for HIV and STI’s (sexually transmitted infections) at least once a year.
According to the Center for Disease Control there are about 20 million new cases of sexually transmitted infections in the United States, every year. The CDC, recommends getting tested every three months if you are sexually active.
Factors such as age and your number of sexual partners play key roles in how often you should be getting tested. When doctors mention “risk factors” surrounding testing, it can sound scary. But these risk factors don’t imply judgement or irresponsible behavior. Doctors asses your “risk” of transmitting infections in a variety of ways, such as your age group, number of sexual partners, or even having a new sexual partner.

If you’re experiencing symptoms of what you think is an STD or HIV, don’t wait until your yearly screening to get tested. STD symptoms vary from pain or burning while peeing to itchy rashes and muscle aches. Symptoms of HIV are similarly wide-ranging and can present in some as flu-like symptoms while others might not experience symptoms at all. If you’re in doubt, go get tested, NovusACS offers free testing and treatment.
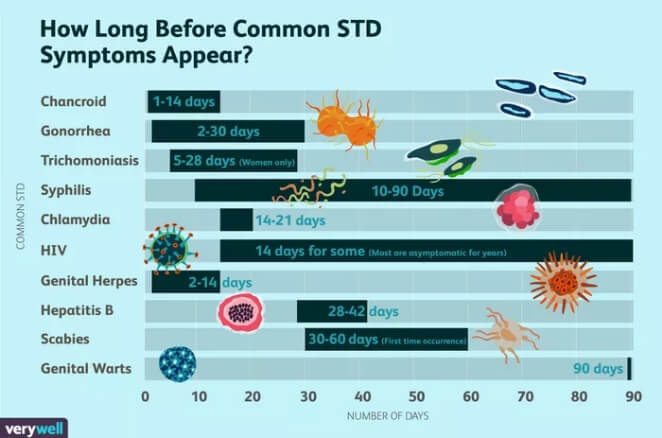
If you’re experiencing symptoms of what you think is an STD or HIV, don’t wait until your yearly screening to get tested. STD symptoms vary from pain or burning while peeing to itchy rashes and muscle aches. Symptoms of HIV are similarly wide-ranging and can present in some as flu-like symptoms while others might not experience symptoms at all. If you’re in doubt, go get tested, NovusACS offers free testing and treatment.
While many STDs are common and the first symptoms may be mild, the consequences of leaving them untreated can be serious. For example, after 10 to 20 years, Syphilis can cause organ damage, paralysis, dementia, and even death. So, ignoring symptoms or hoping they will resolve themselves is not a good idea, especially when syphilis, chlamydia, and gonorrhea can all be completely cured with antibiotics which is available at NovusACS free of charge.
Not all STDs have obvious symptoms and some people may be asymptomatic, or not experience any symptoms at all. Even if you’re asymptomatic you can still pass an STD to your partner and left untreated, your STD could progress and get worse. That’s why regular screenings, coupled with intermittent tests if you’re experiencing symptoms, are so important.
No matter what, if you think you might’ve been exposed to HIV or an STD, get tested, NovusACS offers free testing & treatment. Don’t be afraid to ask questions even if they might be embarrassing. It’s better to have the conversation with a provider than to wonder and suffer in silence. The provider is there to help. If you’re looking to get tested quickly or on a budget, click here to find fast, free testing locations near you.
And remember, frequent testing should NEVER take the place of using condoms. Protection starts with being prepared. To learn more about STD/HIV testing and where you can score PrEP: HIV Prevention and tons of free condoms, click here.







 The following passage from the CDC site regarding U=U applies to both heterosexual men and women and to MSM:
The following passage from the CDC site regarding U=U applies to both heterosexual men and women and to MSM: